ns
Democracy Dies in Darkness
VA reveals sweeping plan to shutter aging
clinics, hospitals in favor of new facilities,
retooled services
By Lisa Rein
March 15, 2022 at 9:00 a.m. EDT
The Biden administration released a sweeping plan Monday to reposition the sprawling
veterans’ health-care system to confront demographic changes and shifts in medicine,
recommending the closure of hundreds of hospitals and clinics and construction of new
ones in areas with greater demand.
Aging hospitals with an excess of unused inpatient beds would close altogether in
communities from Muskogee, Okla., to New York City, and would be replaced by
inpatient and outpatient clinics nearby or new medical centers, with an overall net
reduction of three hospitals. Other medical centers would lose emergency rooms or
surgical services but gain mental health or urgent-care clinics. And new nursing homes
would be built in communities where large numbers of retired veterans are moving.
About 80 new facilities of varying sizes and offering a range of services would eventually
be built.
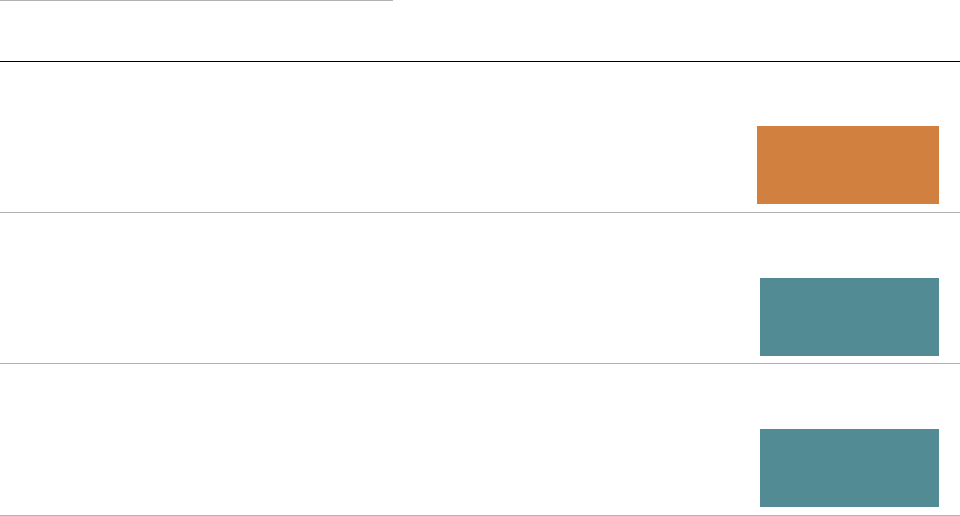
TYPE ▼
CURRENT
FUTURE
CHANGE
VA Medical Center
171
168
−3
−3
−3
Standalone residential
rehabilitation treatment
program
10
22
12
12
12
Standalone community living
center
2
29
27
27
27
Outpatient partnership
0
14
14
14
14
Other outpatient services clinic
255
169
−86
−86
−86
Multi-specialty community-
based outpatient clinic
248
388
140
140
140
Inpatient partnership
7
55
48
48
48
Health-care center
16
30
14
14
14
Community-based outpatient
clinic
555
469
−86
VA chief to recommend hospital closures and expansions in restructuring of the
country’s largest health-care system
Overall, VA’s reliance on inpatient care would taper off as the system catches up to an
outpatient model that private hospitals moved toward decades ago. In many places, the
government-run health-care system’s growing reliance on private doctors and hospital
systems would intensify, picking up where VA would retreat, the recommendations
show.
Lawmakers began poring through the fine print in the lengthy proposal on Monday to
learn what would happen to hospitals and clinics in their districts, while some members
issued defiant statements that previewed the battle to come to stave off reductions in
service to veterans in their districts.
With changes proposed at most of the system’s existing 171 hospitals and 1,112
outpatient clinics, the plan that will be sent to the congressionally mandated Asset and
Infrastructure Review Commission also drew intense interest among veterans groups
and policymakers.
The review mandated by a 2018 law will soon kick off a year of potentially divisive
hearings in affected communities, culminating in a recommendation from President
Biden on which closures should move forward, then a vote in Congress if lawmakers
dislike the proposals. Lawmakers must accept all of the changes or none, and would
have to vote to deny the proposals to stop them. If they take no action, the plans would
take effect. The transformation on the table for Veterans Affairs Secretary Denis
McDonough — while a reconfiguration, rather than a contraction overall — will be
among the most politically sensitive of his tenure.
“Today’s veteran population is vastly different from what it was even five years ago, let
alone decades ago,” Russ Duerstine, deputy director of Concerned Veterans for America,
a group backed by the conservative Koch network, said in a statement. “A rigid system
that cannot adapt to the changing and unique needs of the veterans it serves leads to
waste, complications, and ultimately, an absence of care.”
Duerstine’s group came to prominence during the Trump administration with a
campaign to outsource more medical care for veterans and was instrumental in
muscling the review into the 2018 law, known as the Mission Act, which allowed most of
the 9.2 million veterans enrolled in VA care to see doctors outside the traditional system
of government hospitals.
The restructuring McDonough proposed Monday is driven by changing reality for
veterans, the report said: The Department of Veterans Affairs spends billions of dollars a
year to maintain crumbling facilities that impede doctors from giving veterans the best
possible care, and its hospitals increasingly are located in the wrong places.
Almost 70 percent of VA’s health-care facilities were built more than 50 years ago,
and the buildings have a median age of 60 years — compared with 8½ years for private-
sector hospitals. According to the agency’s budget submission to Congress for fiscal
2022, the health system needs $61.6 billion worth of construction today.
“These facilities were not designed to meet modern health care standards, which limits
VA’s agility and ability to meet evolving Veteran care needs, and basic environment of
care expectations,” the report said.
The population of veterans is declining in the Northeast and parts of the Midwest, and
growing in the South and Southwest, changes largely driven by the aging of those who
fought during the Vietnam era and the increasing loss of those from the Korean War and
the World War II generations. Even though the number of veterans is projected to
decline in coming years, they will need more outpatient and long-term support, such as
nursing home care — and they need more extensive mental health resources than VA
offers.
By 2029 and continuing for a decade, the veteran population will include more women
than ever and will become more racially diverse and younger. VA projects that veterans
will continue to live more in rural areas compared with the rest of the population and
have a higher prevalence of chronic health conditions. All of these shifts “will have
significant effects on health care planning efforts,” the report said. For example, female
veterans, whose numbers are expected to grow by 32.5 percent by 2029 to more than 1
million, need access to gynecological care, mammography and specialized behavioral
health services. “The relative increase in women enrollees may require VA to
significantly increase its capacity to provide sex- and gender-specific care,” the report
said.
While some lawmakers on Monday said they would keep an open mind about the
proposals, others showed early resistance.
Rep. Chris Pappas (D-N.H.) said VA would “jeopardize our veterans’ access to care” with
plans to close three clinics in his rural state.
“Our [clinics] are important community hubs, and I won’t stop fighting to protect
them,” Pappas said in a statement.
Sen. Jon Tester (D-Mont.) took a combative tone on recommendations to close a
nursing home and two clinics in Montana and to change the services offered at two
other locations.
“I will fight tooth and nail against any proposals that blindly look to reduce access to VA
care or put our veterans at a disadvantage,” said Tester, the chairman of the Senate
Veterans’ Affairs Committee, in a statement.
Among Tester’s concerns, and those of other lawmakers who represent rural areas, is
whether enough private doctors exist to take in the potentially large number of new
veterans if VA hospitals or clinics close, congressional aides said.
Even before the plan’s formal release, veterans gathered at a rally in front of the VA
clinic on Staten Island on Sunday with Rep. Nicole Malliotakis (R-N.Y.) and local
elected leaders to protest any closure or realignment of services in the city. Medical
centers in Brooklyn and Manhattan would close, and a clinic on Staten Island would lose
some services to clinics in New Jersey.
Former VA leaders in both parties support the plans, though, calling them a long
overdue, necessary step to keep the system viable.
“We have to move assets where the veterans are now, not where they lived after World
War II,” Robert Wilkie, former president Donald Trump’s second VA secretary, said in
an interview.
“Denis is on target,” Wilkie said of McDonough, acknowledging the political sensitivities
the VA secretary is already confronting. “He is taking on his majority, particularly in the
House.
”
In places where existing hospitals and clinics would close or lose service — in Sturgis
and Hot Springs, S.D.; Chillicothe, Ohio; Leeds, Mass.; Fort Wayne, Ind.; and elsewhere
— the plan does not specify how much care would ultimately shift to alternate providers,
whether those be academic affiliates, clinics run by the Defense Department or private
doctors and hospitals. VA has redirected billions of dollars from veterans’ hospitals to
private health-care providers in recent years in a controversial transformation.
The shift has led to gaps in VA’s own data, a weakness McDonough acknowledged as he
previewed the hospital plan last week at an event hosted by Rand Corp. The
Government Accountability Office (GAO) said in an audit in February that VA lacks
information on key metrics such as the quality of care in the private system, the wait
time for private care appointments compared with VA services, and the relative costs of
each kind of care.
“We found that VA’s approach includes incomplete information on the demand for and
supply of non-VA care, including community care, which is critical to understanding
how best to meet veterans’ future demand for care,” GAO wrote. “The lack of data on
such a key element to VA’s delivery of care may erode confidence in any proposals that
are ultimately forwarded to the Commission.”